A Brief Review of Left Ventricular Diastolic Function and Dysfunction
An introduction to the echocardiographic analysis of left ventricular diastolic function and dysfunction, and noninvasive estimation of filling pressures
January 23, 2021
(updated April 23rd, 2022)
Pages 1 – 18
Table of Contents
- Introduction
- Diastology and diastolic function
- Aims
- Diastolic dysfunction
- Very brief history of the method
- Physiopathology
- Estimation of the determinants of diastolic function
- Estimation of LV filling pressures
- Other factors affecting the noninvasive estimation of LV filling pressures
- The new (2016) EACVI-ASE Recommendations
- Dynamic maneuvers
- Conclusions
- References
Abbreviations
- DD: diastolic dysfunction
- DF: diastolic function
- FP: Filling pressures
- LA: left atrium
- LV: left ventricle
- PCWP: Pulmonary Capillary Wedge Pressure
[see page links at bottom of page]
INTRODUCTION
The analysis of left ventricular (LV) diastolic function (DF) is a complex subject that should not be oversimplified, under penalty of trivializing the complex interactions existing between the blood flows that are sampled with the echo-Doppler examination and the pathophysiological mechanisms that drive the filling and emptying of the heart chambers. Furthermore, it is important to keep in mind that LV DF cannot be completely separated from LV systolic function, since relaxation and contraction are driven by similar mechanisms (Figure 1). This brief practical discussion aims to provide the necessary tools – the physiopathological principles of LV DF and the different available echocardiographic methodologies – and to critically review what is proposed by the current guidelines, with the aim to efficiently use echocardiography (i.e., non-invasive hemodynamics). As recommended by the 2009 EAE / ASE Guidelines (1), “the evaluation of LV DF should be an integral part of a routine examination, especially in patients presenting with dyspnoea or heart failure”. It had been shown in the 80s that – with a comparable severe reduction in systolic function – the LV chamber compliance could be normal or reduced, correlating in this second case with dyspnoic symptoms and worse prognosis (2).
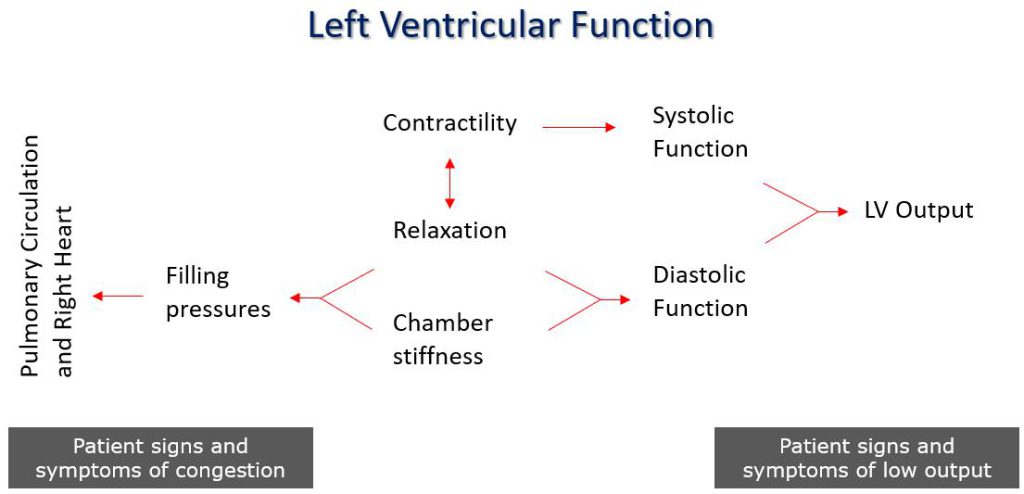
Figure 1. Interaction of left ventricular systolic and diastolic functions.
Cardiac output is the resultant of both systolic and diastolic functions. While mechanical systolic function (eg: ejection fraction) recognizes contractility as the only main determinant, diastolic function recognizes two main determinants independent of each other: LV relaxation and LV chamber compliance (or its reciprocal, stiffness). In this sense, the term “diastolic dysfunction” is relatively imprecise, as it can refer to an isolated alteration of relaxation or of chamber compliance alone, or to an alteration of both determinants. However, the final outcome – once the initial compensation mechanisms have been exhausted – will be an increase in the filling pressures (mean left atrial pressure) needed to overcome the resistance to filling exerted by the increased stiffness of the ventricular chamber, with the aim to maintain an adequate ventricular filling volume and hence cardiac output.
DIASTOLOGY AND DIASTOLIC FUNCTION
Diastology is the science of characterizing the diastolic properties and LV filling pressures (FP) and filling modalities, and their clinical application. In contrast, the LV FP is defined as the ability of the LV to cope with an adequate filling volume in keeping a low ventricular pressure (<12 mmHg). On the other hand, we define systolic function as the ability of the LV to produce a cardiac output adequate to the metabolic needs of the body. The analysis of LV DF in routine echocardiography has also grown following the diagnostic distinction of heart failure with reduced versus preserved systolic function (HFpEF, Heart Failure with preserved Ejection Fraction; HFmrEF, Heart Failure with mid-range Ejection Fraction). To the aim of recognizing this syndrome, the European Society of Cardiology heart failure guidelines have established that echocardiography is sufficient to identify an alteration of LV relaxation or compliance, without resorting to cardiac catheterization, thus “validating” the use of echocardiography in this clinical setting (3). This recognition follows the large number of studies that have been published between the end of the 1980s and the early 2000s, which have validated an array of echocardiographic indices in different patient populations capable of answering the decisive questions of diastology:
1) what is the LV FP ?;
2) by which mechanism did it increase?