TT Pericardial Constriction and Atrial Fibrillation
经胸超声心包缩窄和房颤
Diagnosis of pericardial constriction complicated by atrial fibrillation
心包缩窄合并房颤的诊断
June 4, 2022
Pages 1 – 4
See also in this website the teaching module on: “Pericardial Effusion, Tamponade and Constriction“
亦可见此网站教学模块:“心包积液、填塞、缩窄”。
A 44-year-old patient presented at the outpatient echocardiography laboratory for a follow-up transthoracic echocardiography. Previous CABG, followed by diagnosis of pericardial constriction (post-pericardiotomy). Chronic atrial fibrillation. NYHA II.
The exam shows normal LV end-diastolic volume (38 ml/m2) and biplane ejection fraction (66 %); severe left atrial dilatation (69 ml/m2) (Figure 1); mildly increased estimated pulmonary systolic pressure (40 mmHg) with a dilated inferior vena cava without inspiratory collapse (Figure 3). Moderate right atrial dilatation and mild tricuspid regurgitation. Mild to moderate right ventricular dilatation with normal systolic function.
There are echocardiographic signs which suggest (and confirm) the diagnosis of pericardial constriction.
一位44岁患者到门诊超声心动图室接受经胸心脏超声随访。既往冠脉搭桥病史,后诊断为心包缩窄(心包切开术后)。慢性心房颤动。NYHA II(纽约心脏病学会心功能II级)。
检查显示左室舒张末期容积正常(38ml /m2),双平面射血分数正常(66%);重度左房扩张(69ml /m2)(图1);估测肺动脉收缩压轻度升高(40 mmHg),下腔静脉扩张,无吸气塌陷(图3)。右房中度扩张,三尖瓣轻度返流。右室轻到中度扩张,收缩功能正常。 超声心动图信号提示(并证实)心包缩窄的诊断。
Echocardiographic signs of help for the diagnosis of pericardial constriction:
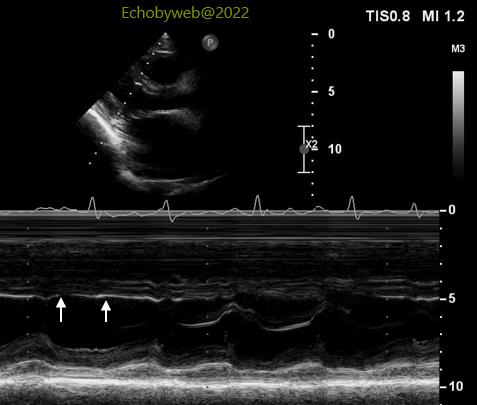
> In the parasternal long-axis view the anterior interventricular septum does not show the typical leftward shift during inspiration (Figure 1) found in patients with significant pericardial constriction, although the m-mode tracing shows a flat septum in diastole (Figure 4, arrows); the septum does not expand towards the right ventricle during diastole, a “minor” sign which suggests a limitation of diastolic LV filling, as in pericardial constriction.
> The dilated inferior vena cava without inspiratory collapse points to an elevated estimated right atrial pressure (combined with right atrial dilatation, Figure 7). This finding is not explained by the mild tricuspid regurgitation. Futher, right ventricular systolic function (Figure 7) and pressure (pulmonary systolic pressure) are respectively normal and mildly increased. Thus, increased RA volume and pressure are not explained by volume or pressure overload on the right side.
有助于诊断心包缩窄的超声心动图信号:
>在显著心包缩窄的患者中发现,胸骨旁长轴视图中,吸气阶段前室间隔不显示典型的向左移动(图1),尽管M模轨迹显示间隔舒张期扁平(图4,箭头处);舒张期间隔不向右室扩张,是提示心包缩窄中舒张期左室充盈受限的“微小”信号。 下腔静脉扩张,无吸气塌陷,指示右房估测压力增加(图7,合并右房扩张)。这种发现不能用三尖瓣轻度返流来解释。右室收缩功能(图7)及压力(肺收缩压力)分别为正常和轻度增加。因此,右房容积和压力的增加不能用右侧心脏压力或容积超负荷来解释。