Bicuspid Aortic Valve & Mild Stenosis
May 29th, 2022
Pages 1 – 5
A case of bicuspid aortic valve with diastolic prolapse, mild stenosis and 3D analysis of stenotic area
See the follo-up pre-CPB TE images here.
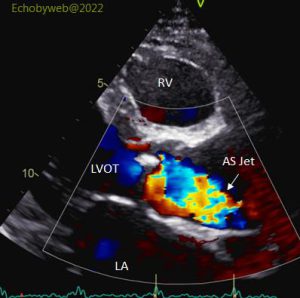
A 72 year old male (BSA= 1.8 m2; HR= 82 bpm; BP= 130/80 mmHg) was admitted because of aortic valve stenosis (Figures 1-3) and dilatation of the ascending aorta (48 mm; ST junction= 32 mm)). LV end-diastolic volume was normal (51 ml/m2), with normal wall thickness and biplane ejection fraction (64 %). Longitudinal systolic function (GE AFI analysis) was reduced (GLS= -14.5 %) (see below). LV filling pressures were estimated normal with grade I diastolic dysfunction. There was mild mitral regurgitation with normal anatomy (PISA method, EROA= 0.1 cm2; regurgitant volume= 18 ml) and the left atrium was moderately dilated (47 ml/m2). There was a mild tricuspid regurgitation with mildly increased estimated pulmonary systolic pressure (40 mmHg).
The aortic valve was bicuspid (Figures 4-5) with a prevalent antero-lateral cusp and a prolapsing postero-medial cusp. There were nodular calcifications. There were no signs of significant stenosis (Max gradient= 26 mmHg, mean gradient= 16 mmHg, valve area at continuity equation= 1.8 cm2; 2D planimetry= 2.3 cm2) (Figure 4), with a mild regurgitation.