TT Gerbode Defect, Acquired
June 26, 2022
Pages 1 – 3
A case of acquired Gerbode defect after surgical aortic valve replacement
A 72-year-old patient underwent open-heart surgery for aortic valve replacement (moderate regurgitation -> mechanical bileaflet prosthesis #24), mitral repair (myxomatous valve with P2-P1 cleft, no prolapse and severe regurgitation), and tricuspid valve repair (moderate to severe regurgitation).
At post-operative transthoracic examination, a high-velocity jet was found arising from the aortic root and expanding in the right atrium, initially mistaken as tricuspid regurgitation suggesting severe pulmonary hypertension and then recognized as an acquired post-operative type 1 Gerbode defect (a communication between the aortic root and the right atrium).
The transthoracic examination shows: atrial fibrillation; normal LV biplane end-diastolic volume (42 ml/m2) and ejection fraction (55 %) (Figure 1); severe left atrial dilatation (103 ml/m2); normal estimated filling pressures (pulmonary regurgitation end-diastolic gradient= 4 mmHg); normal function of the aortic valve bileaflet mechanical prosthesis (mean gradient= 6 mmHg; calculated area at continuity equation= 2.6 cm2) with trace intra-prosthetic residual regurgitation; s/p mitral valve repair (mean gradient= 2.8 mmHg; PHT area= 2 cm2) with trace residual regurgitation; s/p tricuspid valve repair (mean gradient= 0.8 mmHg) with mild residual regurgitation; normal right ventricular systolic function.
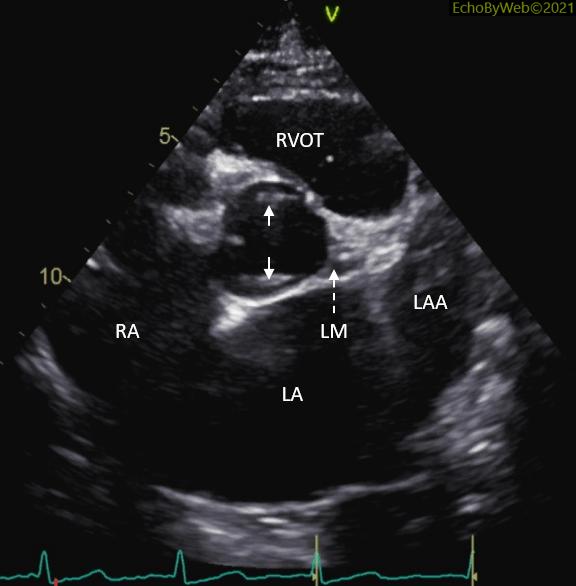
Figure 2 shows the scan at the level of the aortic valve prosthesis with evidence of both a portion of the prosthetic annulus (small white arrows) and of the left main coronary ostium and trunk (LM and white dashed arrow) (Figure 3).
LA: left atrium; LAA: LA appendage; RA: right atrium; RVOT: right ventricular outflow tract.