TT Hypertrophic Apical
May 29th, 2022
Pages 1 – 4
Apical hypertrophic cardiomyopathy diagnosed in the EP department
Post-arrhythmic atrial systolic stunning
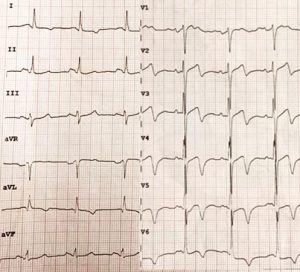
A 57-year-old female (HR= 65 bpm; BP= 130/ 60 mmHg; BSA= 1.73 m2) was admitted in the EP department because of recurrent symptomatic paroxysmal atrial fibrillation. The baseline ECG (Figure 1) showed SR and deep negative T waves in the chest limbs.
The routine echocardiographic examination before the scheduled ablation procedure showed a severely dilated left atrium (86 ml/m2) (Figure 2), nodular calcifications of the posterior mitral annulus, and a reduced LV end-diastolic volume (28 ml/m2) with normal biplane ejection fraction (67 %). There was a mild tricuspid regurgitation and the estimated pulmonary systolic pressure was moderately increased (48 mmHg).
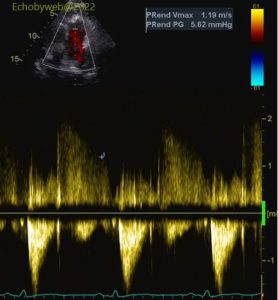

Pulmonary diastolic pressure (and thus LV filling pressure) was estimated as normal, by sampling the pulmonary regurgitation end-diastolic velocity (Figure 3):
Pulmonary diastolic pressure= 5.6 mmHg (end-diastolic gradient) + 6 mmHg (normal inspiratory collapsibility of the inferior vena cava) = 11.6 mmHg.
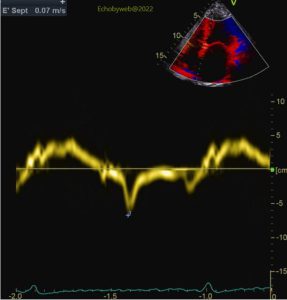
The combined analysis of the mitral valve flow profile (Figure 4) and the tissue Doppler sampling of the mitral annulus (in the 4-chambers view) (Figures 5-6) suggested left atrial systolic stunning (post-arrhythmic: recent spontaneous cardioversion of paroxysmal atrial fibrillation): the E/A ratio is high (2.1) in a 57-year-old patient with normal LV systolic function and filling pressure, and the peak A wave velocity (atrial systolic function) is reduced both at mitral flow velocity sampling and tissue Doppler mitral annulus sampling.