[Page 16]
OTHER FACTORS AFFECTING THE NONINVASIVE ESTIMATION OF FILLING PRESSURES
Age. Age has an important independent influence on all parameters of LV DF that take into account LV relaxation, as the speed of relaxation is maximum in younger subjects (<30 years), and then progressively decreases after age 50 (Table 3). On the other hand, the contribution of LA systolic function (= transmitral A wave) to LV filling is minimal in young patients (<30 years), and then progressively increases as a compensatory mechanism for the physiologically prolonged LV relaxation. As such, the E/A ratio gradually decreases and becomes less than 1 around 60 years, while the E wave deceleration time gradually lengthens (9). It is for this reason that normal values for the LV DF parameters vary with age (Table 3). Age does not directly influence the estimates made with continuous wave Doppler (mitral and pulmonary regurgitation).
Heart rate. Bradycardia and tachycardia have an important independent influence on some of the LV DF parameters. Bradycardia lengthens the diastolic filling time and therefore facilitates LV filling and reduces LV preload, especially in the presence of prolonged LV relaxation. Tachycardia has the opposite effect. Consequently, bradycardia redistributes LV filling towards early diastole increasing the transmitral E wave, lengthening the diastasis phase, and reducing the LA contribution to LV filling (A wave) through the LA Starling’s law, because LA volume will decrease more before reaching LA end-diastole. Conversely, tachycardia will impede LV early filling, redistributing LV filling towards end-diastole, with a reduction of the E wave, elimination of diastasis and an increase in the LA contribution to LV filling (increase in LA preload; LA Starling’s law). A heart rate> 90 bpm causes a “fusion” of transmitral E and A waves, and tissue Doppler E and A waves, and thus the resulting single wave cannot be analyzed. Heart rate affects the pulmonary venous flow profile less and does not directly influence estimates made with continuous wave Doppler (mitral and pulmonary regurgitation).
Left atrial anatomy and function. The LA systolic function is the main extrinsic determinant of LV DF (Table 2): the achievement of an optimal end-diastolic LV filling and cardiac output – and thus an efficient utilization of the LV Frank-Starling mechanism – depends on LA systolic function, paying as little as possible in terms of LV filling pressures. Furthermore, LA pressure (the object of our noninvasive estimation) depends significantly (and reciprocally) on LA chamber compliance (and therefore on the LA volume changes during LV systole), and more indirectly on the LA maximum volume (Figure 8). Finally, several studies have observed that LA dilation is the result of LA remodeling, which reflects a “chronic burden” of cardiovascular pathology and is, therefore, a marker of DD (21).
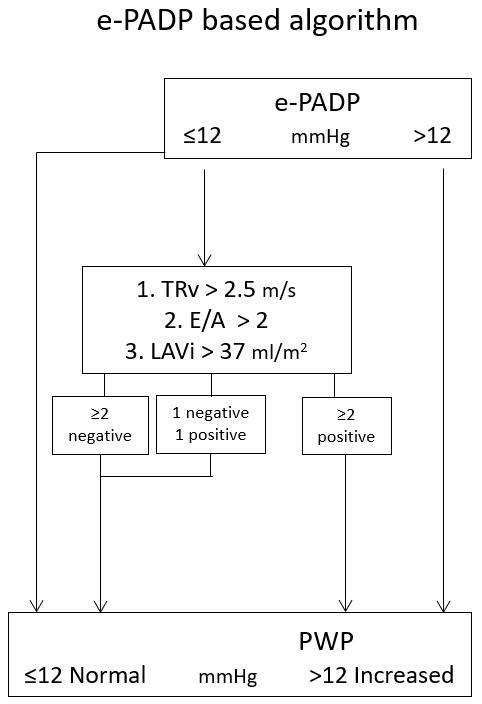
Pulmonary systolic pressure. It is known that pulmonary systolic pressure correlates closely with pulmonary capillary wedge pressure in patients with heart failure (22). Similarly, LV DD has been shown to be an important determinant of pulmonary systolic pressure in patients with primary LV systolic dysfunction.
THE NEW ASE (American Society of Echocardiography) / EACVI (European Association of Cardiovascular Imaging) GUIDELINES
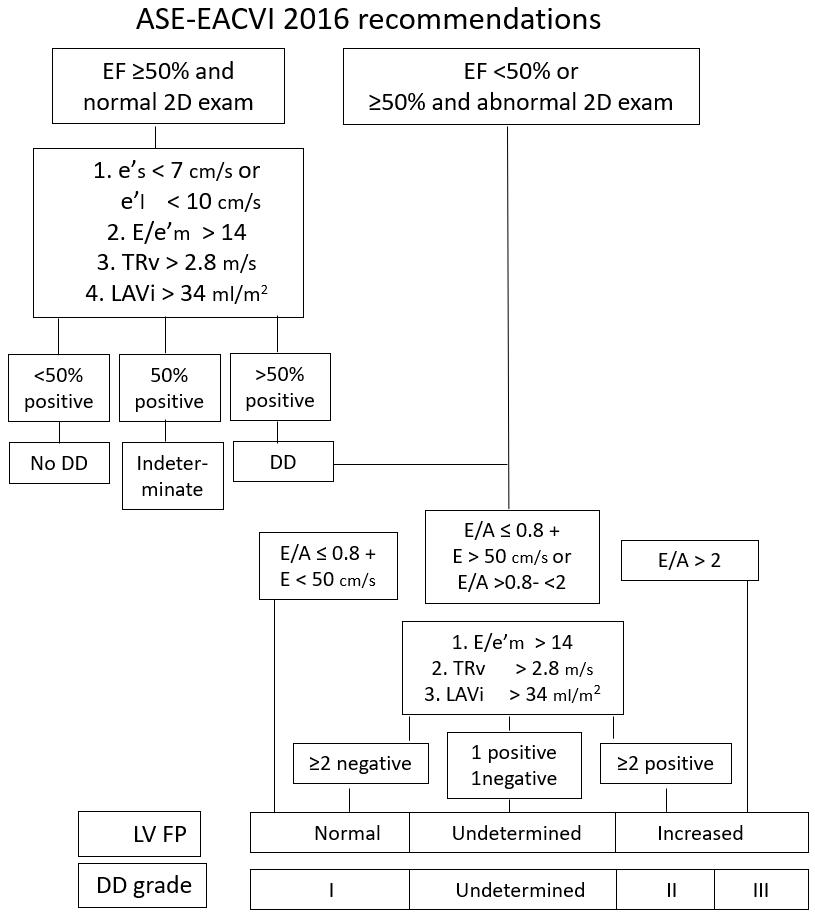
Just as the first joint American and European guidelines (1) defined the analysis of DD and the estimation of LV FP depending on LV ejection fraction – depressed or normal – the new Guidelines make the same distinction (10), proposing differentiated algorithms. The current Guidelines emphasize the need to perform a multiparametric estimate, identifying “fundamental” parameters to be measured simultaneously and using a relative majority selection criteria (Figure 16a). Although originally these algorithms have been proposed by a panel of experts (based on the evidence of the literature) without validation, validation studies have been published in recent years.
• In patients with normal systolic function: to estimate the presence of a DD, the “positivity” of ¾ of 4 parameters is required (E/e ‘ratio> 14; peak septal e’<7 cm / s or lateral e’<10 cm / s; peak tricuspid regurgitation velocity > 2.8 m/s; LA volume index> 34 ml/m2). If ¾ parameters are negative, the FD is estimated normal, otherwise it is defined as “indeterminate”.
• In patients with reduced systolic function: to estimate the presence of DD grade III (associated with increased LV FP), it is sufficient to measure an E/A ratio ≥2, whereas to estimate a DD grade I (associated with normal LV FP), the combination of E/A ≤0.8 + peak E ≤50 cm / s. In intermediate situations of E/A and peak E, the “positivity” of 2/3 of 3 parameters is required (ratio E/e ‘> 14; peak velocity of tricuspid regurgitation> 2.8 m/s; LA volume index > 34 ml/m2) to estimate DD grade II (and associated increased LV FP. If only 2 criteria with contrasting measures are found, the DD is defined as “indeterminate”.