[Page 11]
Echo-guided pericardiocentesis.
- The echocardiographic 2D exam allows the correct identification of location and severeity of the pericardial effusion before pericardial puncture.
- Saline infusion (echocontrast) during 2D monitoring of pericardiocentesis allows to identify the position of the tip of the catheter / needle and thus to reduce the risk of cardiac perforation (Figure 71).
- The monitoring with 2D and Doppler echocardiography allows to identify regression of tamponade and hemodynamic normalization, and to identify any residual effusion.
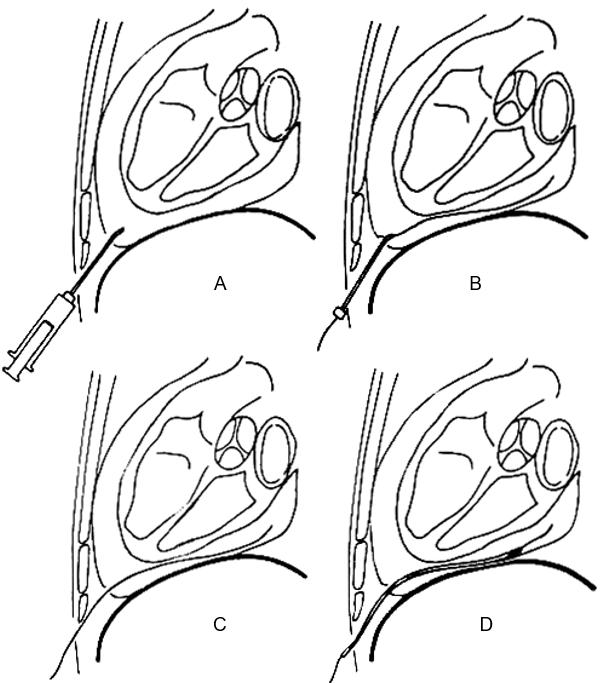
Susini G et al. Percutaneous pericardiocentesis versus subxiphoid pericardiotomy in cardiac tamponade due to postoperative pericardial effusion. J Cardiothorac Vasc Anesth 1993;2:178.
Figure 73-75. Severe pericardial effusion and tamponade before pericardiocentesis (Fig. 73); complete systolic collapse of the RA is seen. Resolution of tamponade during pericardiocentesis (Fig. 74): no collapse of the RA wall (only systolic contraction). Fig 75: residual effusion post-pericardiocentesis.

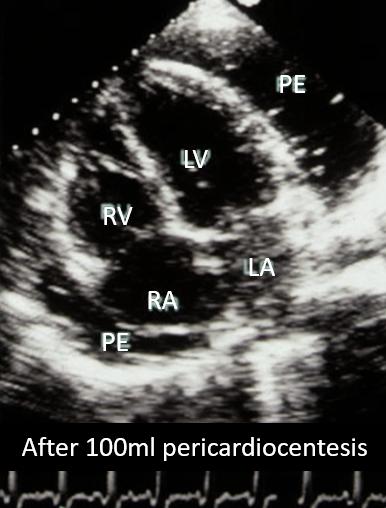
Figures 76-77. Resolution of complete RA wall collapse (Fig. 76, double white arrow) after initial drainage of 100 ml with pericardiocentesis (Fig. 77). Residual large effusion (PE).
Mayo Clinic experience (Tsang et al, Chest 1999;116:322).
- 245 echo-guided pericardiocentesis
– Thoracic wall= 86%
– Subcostal 12%
– Not documented 2% - Echocardiography necessary for diagnosis (aspecific sings/symptoms)
- Therapeutic success 97%
- Urgencies 39%
- Tamponade: 70%
- TE necessary in 1%
- Post-pericardiotomy syndrome: 31%
- Major complications: 2% (2 cardiac ruptures (surgical repair, 3 pneumothorax)
- Similar failures for circumferential and loculated effusions
- 1% of constrictions after 2 years F-U
- Reduced risk of recurrences with pericardial catheter
- Predisposing factors: a) anticoagulants; b) post-pericardiotomy syndrome
- Mortality related to effusion: 1% (late tamponade)