What a Difference a Slow Flow Makes?
The hemodynamics behind the mitral valve E wave and prolonged LV relaxation.
April 20, 2022
Pages 1 – 2
Topics:
- Noninvasive hemodynamics
- Left ventricular diastolic function
- Left ventricular prolonged relaxation
- Left ventricular compliance
- Left ventricular and left atrial pressure
- Mitral valve flow
- Pulsed Doppler Mitral E and A wave
- Stroke volume
[A brief Review of LV diastolic function and dysfunction can be found here in the website].
The recently published 2016 ASE-EACVI Recommendations for LV diastolic function (1) have put some order in the confusing arena of LV diastolic function evaluation with echocardiography by publishing flow charts that guide the use of the multiple tools that we use in everyday routine work.
However, the use of these Guidelines relies on the understanding of the basic information provided by each of the tools that we use: pulsed Doppler / continuous wave / tissue Doppler imaging of mitral valve / pulmonary venous / pulmonary regurgitation / mitral annulus dynamics. The first step is a comprehensive utilization of the hemodynamic information provided by the analysis of pulsed Doppler mitral valve flow velocities.
Let’s have a look at the information that we can “extract” from a mitral valve flow velocity profile (MVF).
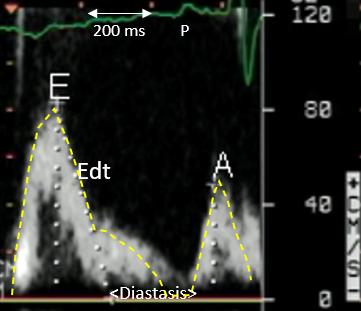
Figure 1. This MVF is from a relatively young subject (< 50 y.) with a heart rate= 71 bpm. Age and heart rate are the first important variables to consider when evaluating MVF. MVF changes with age (2) mainly because ageing prolongs significantly LV relaxation, and the latter is one of the main determinants of the early diastolic E wave of MVF . Heart rate modifies to a greater extent than age the MVF by prolonging (bradycardia) and shortening (tachycardia) the diastolic filling period.
In our case, a heart rate= 71 bpm is sufficiently slow to allow for a complete LV relaxation, demonstrated by a deceleration slope (Edt) which reaches rapidly the baseline (white dots). After that, some LV filling continues during diastasis, until atrial contraction completes the LV filling allowing – through the Frank-Starling relationship – to reach an optimal stroke volume.
Coming back to the first 1/3 of diastole, LV relaxation and the simultaneous early diastolic E wave velocity, we can infer from our flow velocity profile that LV relaxation in our subject is normal, since we can observe:
1. a relatively high peak E wave velocity= 80 cm/s with a concomitant long E wave duration (> 200 ms), the combination of which determines a physiologic prevalent early diastolic LV filling, driven by the normal LV relaxation;
2. a normal E wave deceleration time; in this young patient Edt= 160 ms, which points to a fast relaxation (in contrast to a rapid increase in LV early diastolic pressure secondary to reduced LV compliance); this observation points to the importance of taking into consideration the patient’s age before considering any LV diastolic function measurement.
3. a small atrial contraction (A) wave, determined by the fact that the left atrium has emptied into the LV mostly during early diastole, and only a small amount of LA volume is left to be driven by atrial systole into the LV in end-diastole.
This flow pattern is characteristic of a combination of normal LV relaxation (and thus of a younger age or older age but athlete), a heart rate < 80 bpm, and a normal stroke volume.
This leads to the observation that MVF can tell us a lot about stroke volume, since what transits through the mitral valve in diastole must also – in the following beat and in the absence of mitral regurgitation or ventricular septal defect – transit through the aortic valve. Stroke volume is the product of the total mitral velocity-time integral x mitral annulus area. When – as in Figure 1 – the E wave represents most of the total mitral velocity-time integral (the yellow dashed line), then we can consider the “area” of the E wave as a visual surrogate of stroke volume, which in this case is normal. In the absence of mitral regurgitation, a large E wave is synonymous with a healthy LV (normal diastole and stroke volume). So, it is important to keep an eye on the time markers of our pulsed Doppler tracings, so to have an idea of how long is the duration of diastole and more so how long is the duration of our E wave.
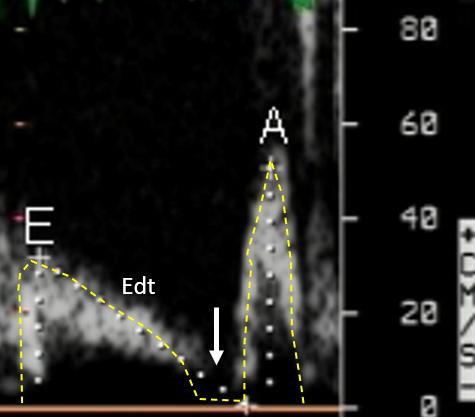
Figure 2. In striking contrast, this older (> 60 y.) patient shows a quite different MVF. Heart rate is similar, but the diastasis phase is absent (white arrow) because the whole of early and mid diastole is occupied by the deceleration of the E wave (Edt) with a very long deceleration time (420 ms) which is diagnostic of a (pathologic) prolongation of relaxation. The peak E wave is also quite small (around 30 cm/s), which is also consistent with a slow deceleration of the LV pressure fall during isovolumic relaxation which in its turn reduces the early diastolic pressure difference between the left atrium and the left ventricle. Since pulsed Doppler velocities are produced by the local pressure gradients, then
reduced pressure gradient = reduced peak velocity.
In this case the E wave has a long duration, but unlike our normal subject in Figure 1, it is associated with a pathologic Edt (and a small E wave velocity-time integral).
The (relatively small) increase in the A wave (to almost 60 cm/s) marks a shift of stroke volume from early to late diastole (Figure 2), and determines the inversion of the E/A which has a positive value in normal young subjects. Since LV relaxation is markedly prolonged (impaired), at the end of the first 2/3 of LV diastole(white arrow) a larger amount of blood – compared to the normal subject of Figure 1 – is left in the left atrium, and must be transferred to the LV during atrial systole in order to maintain the stroke volume. This is the “compensatory role ” of atrial systole in the setting of LV prolonged relaxation. If this mechanism fails, then stroke volume declines.